The use—and disposal—of personal protective equipment (PPE), syringes and other health care products have been top of mind during the coronavirus pandemic, lending new urgency to the efforts of hospitals and other entities to keep medical waste from becoming a landfill casualty.
Efforts to find new life for masks, gowns, tubing and all the other plastic equipment needed to fight disease and treat patients’ injuries run the gamut—strategies include recycling, depolymerizing, even refurbishing some limited-use devices.
Because of the burdens of collecting, sorting and storing waste traditionally deemed hazardous, hospitals face a significant challenge to recover value from such items, says Christopher Bodkin, data coordinator for sector performance and recognition for Practice Greenhealth, a Reston, Virginia-based nonprofit network of about one-third of the hospitals in the U.S. and Canada that’s working to combat waste.
Among those hoping attention on medical waste leads to changes is Dan Vukelich, president and CEO of the Association of Medical Device Reprocessors (AMDR), Washington, which works to extend the usable life of some medical equipment throughout the world, mostly in the U.S.
“With COVID having shone the light on the vulnerabilities of the health care supply chain, I think our issue has gained tremendous attention,” he says. “You don’t have to change your purchasing patterns; you can continue to use the devices you like, but we can help extend their lifespan, so you don’t have to buy as much or contribute so much waste or emissions.”
Mayo Clinic crafts its own Rx
The Mayo Clinic, which treats about 1 million patients a year at locations throughout the world, is one of many hospitals confronting the waste-reclamation challenge.
“Approximately 30 percent of the waste stream was recycled in 2021,” says Amanda Holloway, director of the Office of Sustainability for Mayo. “The overall waste stream is comprised of municipal solid waste, regulated medical waste, as well as hazardous waste items common to health care operations. Waste is disposed of in a variety of ways, including waste-to-energy, incineration and autoclave.”
Since 1990, Mayo has operated its own recycling center near its flagship campus in Rochester, Minnesota, where it processes an average of 5,500 tons of material each year, such as paper, cardboard and a variety of plastics, “including plastics from laboratories, patient care and surgical areas,” says Glen Goodsell, Mayo recycling coordinator.
Goodsell says the pandemic has increased consumption of one plastic product in particular—the expanded polystyrene (EPS) coolers used to transport COVID-19 testing supplies. Mayo densifies EPS on-site after use, then cuts the densified logs for transport to a recycler off-site; last year, it recycled 110 tons of EPS.
It handles plastic items made from No. 5 rigid polypropylene (PP) in a similar manner—grinding it on-site and selling the flakes for reuse, Goodsell says.
Vital statistics
Mayo is no outlier in generating waste, including water pitchers, water bottles and caps, syringe cases, pipette tip containers and surgical trays.
The experiences of the U.K.’s National Health Service (NHS) are illustrative. According to a recent report available from Safetec Direct, a supplier of safety equipment, including PPE, in the U.K, NHS hospitals used around 748 million PPE items over the course of just 53 days early in the pandemic. The items included 470 million gloves, 145 million aprons, 132 million masks and 1.2 million gowns.
One study found that 69 percent of all waste found on British beaches at one point was PPE.
Practice Greenhealth, which provides recommendations to health care organizations looking to rein in waste or adopt more-sustainable practices, has tracked trends that show the overall problems with waste are only growing.
From 2000 to 2019, the amount of plastic waste doubled, Bodkin says.
In the U.S., the Healthcare Plastics Recycling Council, Shoreview, Minnesota, has found health care facilities generate about 1.17 million tons of medical waste annually, Bodkin says.
That includes about 29 pounds of waste per bed per day, contributing a total of about 5 million pounds of waste per year, according to Practice Greenhealth. Blue wrap—the nonwoven PP used to wrap surgical tools—makes up 225 million pounds of waste per year. By itself, Mayo uses 35 million pounds of the stuff annually, Goodsell says.

Contributing causes
Internal and external logistics pose challenges for hospitals that set out to recover all that waste, Bodkin says.
Traditionally, end-of-life products that have been used in health care settings have been viewed as hazardous materials, no matter how they were used originally, he says. Most end up at a landfill, while some of the waste materials are incinerated.
Most medical products aren’t designed for recyclability, and because of concerns about sterility, even products that could be reused often aren’t, he says.
“All hospitals would like to do this, but the first thing they talk about is, ‘We need to train our staff. We need to figure out where to store this stuff’ or ‘We have no room to store it, so it needs to be picked up every day,’ which creates its own financial and sustainability equation,” Bodkin says.
Accumulating enough waste of any one material valuable enough to ship to a recycler is another difficulty, especially for hospitals in locations with poor recycling infrastructure—areas Bodkin calls “recycling deserts.”
Better off blue

GreenMantra Technologies is one company looking to fill roles mechanical recycling can’t.
As part of a research project funded by the Canadian government, the company, which transforms hard-to-recycle plastics into specialty waxes, showed it could effectively handle medical masks.
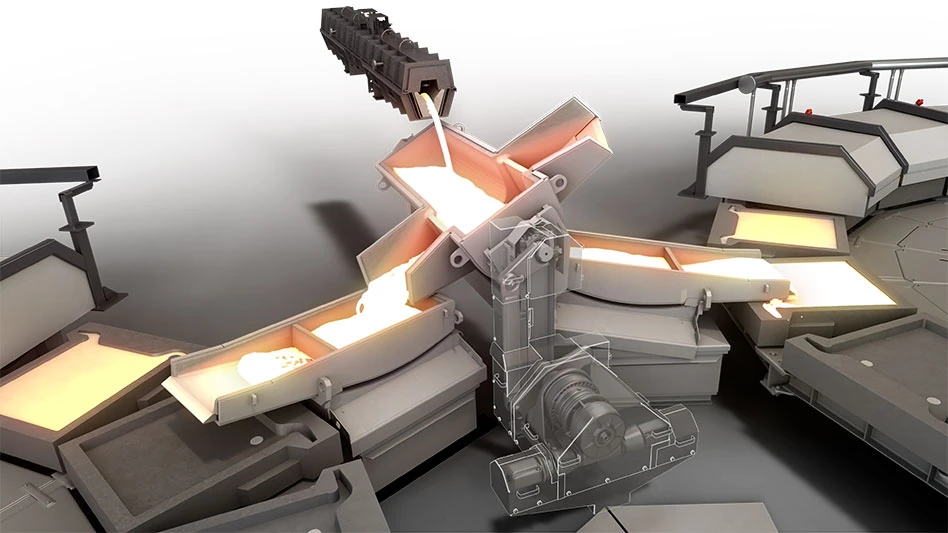
GreenMantra’s proprietary reactors, which depolymerize plastic using high heat and solvents, recovered value from the material, while leaving one particular characteristic intact—the blue color used to make many masks.
“We were producing a bluer wax as a product of that, but we had full confirmation from our customers that it was still our high-quality polypropylene-based wax that could be used in our applications,” says Ben Scott, director of technology.
A specialty chemical company, Brantford, Ontario-based GreenMantra began depolymerizing polyethylene 12 years ago; it has since established processes for PP and polystyrene, and it makes thousands of pounds of waxes per year. Depending on the feedstock, the waxes can be used to enhance the properties of materials used in asphalt and roofing applications, Scott says.
“We strive for zero-waste, obviously,” he says. “We have a little bit, but we have a pretty solid mass recovery. ... We’re at about 93 to 95 percent mass recovery.”
For GreenMantra, medical waste presents an opportunity.
“We will be looking to source as much of this material as possible because it’s a reasonably high-grade polypropylene material, which shouldn’t end up not being recycled,” Scott says.
Ready for reuse
While GreenMantra is producing waxes, AMDR has found a way to keep medical devices in circulation by reprocessing them according to U.S. Food and Drug Administration (FDA) standards.
“Everything has to be disassembled, cleaned, put back together, tested, inspected [and] repackaged, and then everything is sent out sterile or disinfected, depending on its level of criticality, according to the same standard that applies to the original manufacturer,” Vukelich says. “And then it’s sent back to the hospitals.”
The process addresses one vexing issue faced by hospitals trying to recover value from plastics—a concern over contamination that has pushed facilities to increasingly purchase disposable devices.
“As plastics became easier to produce and cheaper to purchase, and more products came online, many reusable devices in the health care setting, where they used to be autoclaved, cleaned and reused, switched over to single-use plastic devices,” Bodkin says. “And that was mainly because of the economics. But there is also the general and rightly placed fear of sterility when working in the health care setting that has further pushed more and more products to be made from single-use plastics.”
But reuse can be a safe and cost-effective alternative to the use-and-toss cycle, Vukelich says.
Along with medical device OEMs, AMDR, which operates eight facilities throughout the U.S., cleans and tests devices that are shipped from hospitals for recertification by the FDA. Each device is tracked and traced and used as many as three times—the limit established by the FDA.
Device OEMs, reprocessors and many hospital systems, including blue-chippers like Mayo and the Cleveland Clinic, are among AMDR’s members. Hospitals benefit from the program because they can buy back devices at a savings of up to 40 percent off what new devices would cost, Vukelich says.
Devices suitable for reprocessing include common hospital paraphernalia, such as pulse oximeters and blood-pressure cuffs, as well as more sophisticated products, like ultrasonic scalpels, which cost about $400 brand new, and diagnostic catheters, which cost $2,000.
“The business model that reprocessors employ, we recover devices that have a price point where it’s expensive enough that it’s worth investing all the R&D or reverse-engineering, the research and development to reprocess them in a way that they’re going result in [being] safe and effective, and there’s enough life in them, meaning they’re durably built enough that you can get multiple uses,” Vukelich says.
“With COVID having shone the light on the vulnerabilities of the health care supply chain, I think our issue has gained tremendous attention. You don’t have to change your purchasing patterns; you can continue to use the devices you like, but we can help extend their lifespan, so you don’t have to buy as much or contribute so much waste or emissions.” — Dan Vukelich, president and CEO of the Association of Medical Device Reprocessors
Untapped potential
Coming out of the pandemic, Vukelich has hope hospitals and outside organizations will continue to make strides to address medical waste.
“I do think there’s going to be increased attention in hospitals,” he says. “I do think there’s going to be increased attention from regulators to buy more sustainable or longer-lasting products.”
As GreenMantra and AMDR can attest, material that would otherwise be dumped or burned has value, and Scott says GreenMantra is eyeing expansion beyond Canada to locations that include the U.S.
Meanwhile, Vukelich is hoping to win work with the U.S. Veterans Administration, one of the few big health care systems with which AMDR doesn’t already partner. He believes the association’s efforts could save the U.S. health care system billions of dollars.
“We think our example has sort of identified a lot of low-hanging fruit. We’re already saving ... hospitals half a billion dollars by taking advanced surgical instruments out of the garbage and putting them into the circular economy stream,” he says. “We only think we’re doing a fraction of what’s possible.”
Hospitals in the U.S. realized most of the savings, but AMDR also has uncovered advantages for hospitals overseas.
In 2020, it handled 11.9 million pounds of material. That is just scratching the surface, Vukelich says.
“I think it’s fair to say that we could more than double that,” he says.
Get curated news on YOUR industry.
Enter your email to receive our newsletters.
Explore the Summer 2022 Plastics Recycling Issue
Check out more from this issue and find your next story to read.
Latest from Recycling Today
- Fenix Parts acquires Assured Auto Parts
- PTR appoints new VP of independent hauler sales
- Updated: Grede to close Alabama foundry
- Leadpoint VP of recycling retires
- Study looks at potential impact of chemical recycling on global plastic pollution
- Foreign Pollution Fee Act addresses unfair trade practices of nonmarket economies
- GFL opens new MRF in Edmonton, Alberta
- MTM Critical Metals secures supply agreement with Dynamic Lifecycle Innovations